Image-guided radiation therapy (IGRT) and radiation treatment accuracy
By Christina L. Mershell
Share:
Precision medicine is a term used often to refer to treatments that are personalized and tailored to an individual with the goal of being the most effective for their cancer diagnosis. In the world of radiation therapy for cancer, there are many ways that treatment can be personalized, as well as focused within a millimeter of the cancer target. Now that’s precise!
What is a millimeter? A millimeter can easily be seen as the width of the tip of a sharp pencil or the tip of a sewing needle. That is really small. Yet when it comes to radiation, it is imperative that radiation is focused on the cancer and not on healthy parts of the body near the cancer.
One way that radiation can be focused on the cancer is the use of proton radiation therapy. Another is the use of Image-Guided Radiation Therapy (IGRT).
Acronyms abound when you are thrown into the world of a cancer diagnosis, medical tests and cancer treatments. When it comes to radiation treatments, this is no exception: RT, IMRT, IGRT, IMPT, PT, CBCT, EBRT, SBRT and so many more.
While this can be confusing, what is not confusing is the fact that you want your cancer radiation treatment to be accurate and precise. In this blog, we will discuss how millimeter precision is achieved through Image-Guided Radiation Therapy (IGRT) with proton therapy.
Definitions of acronyms used frequently by physicians and radiation professionals:
- RT – radiation therapy
- CT - computed tomography scan (also known as a “CAT scan”)
- MRI - magnetic resonance imaging
- IMRT – intensity modulated radiation therapy
- IGRT – image-guided radiation therapy
- IMPT – intensity modulated proton therapy
- PT – proton therapy
- CBCT – cone beam CT scan
- EBRT – external beam radiation therapy
- SBRT – stereotactic body radiation therapy
Proton Therapy
Proton beam therapy is a targeted form of cancer treatment that deposits the highest dose of radiation where it stops in the body. Once the proton radiation stops, there is no more radiation deposited in the body.
While there is some radiation deposited along the path to the target in a person’s body, the dose can be delivered from 360 degrees around the person so that the path of radiation goes through the area that will have the least amount of damage on surrounding healthy tissue—leading to less side effects.
For a refresher course on how proton beam therapy works, read, “What is the difference between proton radiation and radiation therapy?”
Proton radiation therapy uses a beam of protons, which are subatomic particles, that are sent along a beam path at a speed that will deposit the proton radiation at the desired spot in the body. This stopping is considered the “Bragg peak,” which is only a few millimeters wide. Tumors are typically larger than a few millimeters, so the proton beam expands to its target by using an expanded or spread-out Bragg peak. The goal is to cover the entire tumor with this method.
Click here for an image of the Bragg peak and how the proton beam can be expanded to cover the entire tumor.
Patient Positioning
The next step to ensuring millimeter precision of radiation treatment is ensuring that the patient is lying in the same position on the treatment table every day. A patient’s treatment plan is created using imaging, like CT or MRI scans. This happens during a simulation scan before starting radiation.
During simulation scans, radiation therapists determine the ideal position of the patient’s body to ensure that the radiation beams will be able to easily reach the target area as well as to identify the easiest way to reproduce the position of the patient each day during treatment.
The team saves detailed notes in the patient chart during simulation about the position of the patient's body. Then each day during treatment, the medical team aligns the patient in the same exact way.
To accomplish this positioning, patients have custom-made immobilization devices. The positioning devices ensure patients are repositioned correctly before treatment. For example, prostate cancer patients will have an immobilization device uniquely crafted for the lower half of their body, so that the patient’s legs, pelvis, hips and abdomen are in the same anatomical position as the simulation scan. Likewise, if the doctor needs to treat the brain, head, or neck, they make a custom mask for the patient. The mask is then placed on the treatment table for radiation treatment accuracy.
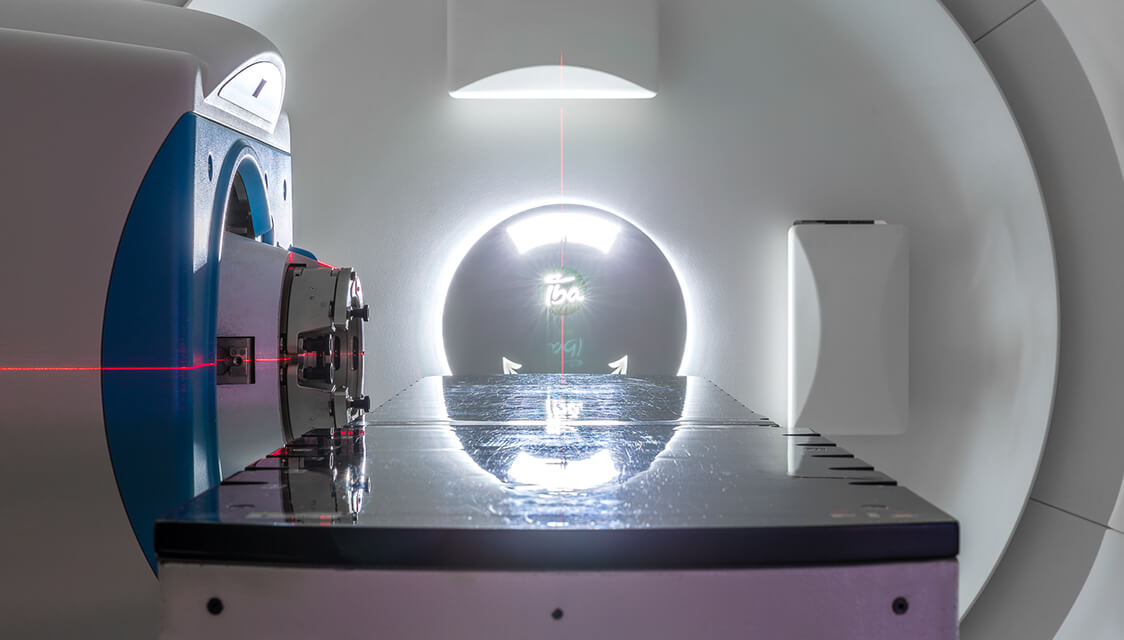
Patients may also have stickers placed at various places on their body to assist with alignment before treatment. The treatment room also has lasers that help ensure accurate patient alignment.


Image-Guided Radiation Therapy (IGRT)
Once the patient is aligned to the external markings according to the specifications set during the simulation scan and the requirements of the cancer treatment plan, it is next time to ensure that the patient is set up accurately from an internal point of view.
Thanks to advancements in radiation treatments, imaging systems are now a part of the treatment room. Most treatment rooms are equipped to take an X-ray or a CT scan of the patient on the table. Radiation therapists take the images of the patient in their treatment position. The scan is then evaluated to the treatment plan, allowing the radiation therapists to determine the small adjustments needed to be made to the patient’s position to ensure alignment with the treatment plan. The image guidance allows the medical team to be as precise as possible for every treatment.
Millimeter Precision Achieved
Thanks to advancements in radiation treatments, including proton beam therapy, the pencil beam scanning method of delivering the proton beam, advanced patient positioning systems and the ability to image the patient immediately before radiation treatment is delivered, millimeter precision in radiation treatments can be achieved.
The accuracy of computer systems and the daily calibration of equipment, lasers and proton beams are important. They help provide some of the most precise radiation treatments for cancer patients today.
Find out more about advancements in proton beam radiation for prostate cancer, head & neck cancers, lung cancer and pediatric cancers on our blog page.


